Review What is special about the tubing used for administration of blood products?
Kinh Nghiệm Hướng dẫn What is special about the tubing used for administration of blood products? Mới Nhất
Hà Trần Thảo Minh đang tìm kiếm từ khóa What is special about the tubing used for administration of blood products? được Update vào lúc : 2022-11-15 11:46:05 . Với phương châm chia sẻ Mẹo về trong nội dung bài viết một cách Chi Tiết Mới Nhất. Nếu sau khi Read tài liệu vẫn ko hiểu thì hoàn toàn có thể lại Comment ở cuối bài để Tác giả lý giải và hướng dẫn lại nha.Chapter 8. Intravenous Therapy
Nội dung chính Show- Checklist 75: Pre transfusion PreparationChecklist 76: Transfusion of Blood and Blood ProductsChecklist 77: Managing a Blood or Blood Product Transfusion ReactionCritical Thinking ExercisesAttributionsWhy is filtered tubing used during infusion of blood products?Can you use the same tubing for blood?How often must you change the tubing for blood products?
All healthcare practitioners who administer blood or blood products must complete specific training for safe transfusion practices and be competent in the transfusion administration process. Always refer to your agency policy for guidelines for preparing, initiating, and monitoring blood and blood product transfusions. These guidelines apply to adult patients only.
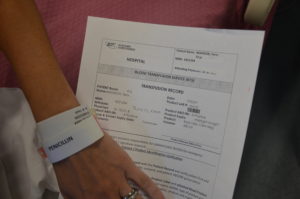
The transfusion of blood or blood products (see Figure 8.31) is the administration of whole blood, its components, or plasma-derived products. The primary indication for a red blood cell (RBC) transfusion is to improve the oxygen-carrying capacity of the blood (Canadian Blood Services, 2017a). An order from a healthcare provider is required for the transfusion of blood or blood products. RBC transfusions are indicated in patients with anemia who have evidence of impaired oxygen delivery. For example, individuals with acute blood loss, chronic anemia and cardiopulmonary compromise, or disease or medication effects associated with bone marrow suppression may be candidates for RBC transfusion. In patients with acute blood loss, volume replacement is often more critical than the composition of the replacing fluids (Canadian Blood Services, 2017a). Transfusions can restore blood volume, restore oxygen-carrying capacity of blood with red blood cells, and provide platelets and clotting factors. The most common type of blood transfusion is blood that is donated by another person (allogeneic). Autologous transfusion is the transfusion of one’s own blood (Perry et al., 2022).
 Figure 8.31 Red blood cells and blood IV tubing. Note the filter is the bottom half of the drip chamber
Figure 8.31 Red blood cells and blood IV tubing. Note the filter is the bottom half of the drip chamber
Transfusion therapy is considered safe, and stringent precautions are followed in the collection, processing, and administration of blood and blood components. However, transfusions still carry risks such as incompatibility, human error, and disease transmission, and blood transfusion must be taken seriously all times. Incompatibility can be decreased by using irradiated red blood cells or leukocyte-reduced blood. The majority of blood transfusion complications are a result of human error (Perry et al., 2022).
Compatibility testing is vital for all recipients of blood or blood products. Recipients must be transfused with an ABO group specific to their own blood type or ABO group-compatible. There are three types of blood typing systems: ABO, Rh, and human leukocyte antigen (HLA). For more information on these, refer to the online resources the end of this chapter. It is vital to understand what types of blood groups are compatible for transfusions (Canadian Blood Services, 2017b).
When administering blood and blood products, it is important to know the patient’s values and beliefs regarding blood products. Some groups of individuals, mainly Jehovah’s Witnesses, may refuse blood transfusions or blood products based on religious beliefs. These individuals sometimes refuse transfusion of whole blood and primary blood components but may accept transfusion of derivatives of primary blood components such as albumin solutions, clotting factors, and immunoglobulins. Always assess each individual’s preference to establish if a blood component is an acceptable treatment to manage their illness or condition (Canadian Blood Services, 2017a).
When managing blood transfusions, it is important to identify issues promptly to manage reactions effectively. Transfusion reactions (mild to life-threatening) may occur despite all safety measures taken. All transfusion reactions and transfusion errors must be reported to the agency’s transfusion medical services (TMS, a.k.a. the “blood bank”). It is imperative to know what signs and symptoms to look for, and to educate your patient on what to report and when to report potential transfusion reactions. Mild to severe reactions may include the following (Canadian Blood Services, 2017b):
- Temperature ≥ 38.0°C or change of 1°C from pre-transfusion valueAcute or delayed hemolytic transfusion reactionHypotension/shockRigorsAnxiety
Back or chest painNausea/vomitingShortness of breath (dyspnea)HemoglobinuriaBleeding/pain IV siteTachycardia/arrhythmiaGeneralized flushingRash ≥ 25% of bodyUrticaria and other anaphylaxis reactionsHemolysis after transfusionCytopenias after transfusionVirus, parasite, and prion infectionsNon-immunological reactions including infectionCirculatory overloadHypothermia
It is important to note that some reactions can occur one or more days after a transfusion (Canadian Blood Services, 2017b). As such, patients going home after a transfusion require education about what to watch for and what do do in the sự kiện of a reaction. For more information on types of reactions, signs and symptoms, and treatments, review the article adverse events related to blood transfusions, or see the online resources the end of this chapter. If patient has a blood transfusion reaction, always follow agency policy to manage mild to severe blood reactions. This text will cover pre transfusion preparation (Checklist 75), transfusion of blood
and blood products (Checklist 76) and then managing a blood transfusion / blood product reaction (Checklist 77).
The steps in Checklist 75 must be completed before obtaining the blood or blood product from the blood bank (Alberta Health Services, 2015a, 2015b; Perry et al., 2022; Vancouver Coastal Health, 2008).
Checklist 75: Pre transfusion Preparation
Disclaimer: Always review and follow your agency policy regarding this specific skill. Safety considerations:- Some blood products require refrigeration. Complete the preparation BEFORE calling for delivery of the blood / blood product.If the product does require refrigeration and cannot be administered immediately, return it to TMS (transfusion medical services) for safe storage.If there is any discrepancy between patient information, group and screen, product ordered, etc., do not
proceed. Stop and verify any discrepancies.Be diligent when preparing to infuse blood. Distractions may lead to errors when verifying information.
 Physician
orders for a blood transfusion
2. Verify the prescriber’s orders for any pre- or post-transfusion medications to be administered.
Medications given prior to transfusion are only considered for persons with documented moderate to severe reactions. Typically medications are administered 30 minutes prior to the transfusion. Examples of meds might include diphenhydramine, acetaminophen, and furosemide.
Physician
orders for a blood transfusion
2. Verify the prescriber’s orders for any pre- or post-transfusion medications to be administered.
Medications given prior to transfusion are only considered for persons with documented moderate to severe reactions. Typically medications are administered 30 minutes prior to the transfusion. Examples of meds might include diphenhydramine, acetaminophen, and furosemide. Remember: These medications can also mask a potential reaction.
3. Obtain the patient’s transfusion history, and note any known allergies and previous transfusion reactions. Past complications may require patient to have pre- and post-transfusion medications to prevent further transfusion reactions. 4. Check that the correct patient facility identification and TMS identification band are on the person.If no facility identification band, apply one.
If no TMS (a.k.a. blood band) present, STOP. Notify TMS.
If any discrepancies STOP. Do not proceed until the discrepancy is resolved.
Group, screen, and cross match must be completed within 96 hours of the transfusion to establish any new antibody formation and to ensure current compatibility.If group and screen are outdated, initiate processes for new testing.
Only TMS can apply blood product related bands.
5. Establish IV site or verify patency of current site. IV sites must be patent and without complications.Blood and blood products cannot be mixed with IV medications. If necessary, establish a site specifically for the blood product.
The IV cannula must be large enough to allow flow of product the correct rate. Generally for adults 20 to 22 gauge. Large cannulas are necessary for rapid infusion (i.e., 16 or larger).
 Assess patency of IV site
Assess patency of IV siteCVCs with multiple lumens may allow blood or blood products to be given simultaneously when medications and other solutions infuse through separate lumens.
6. Verify correct infusion equipment. Prime an IV line following Checklist 66.Initiate primary IV @ 30 cc/hr.
Ensure a back up line of 0.9% NS with a standard IV administration set is available the bedside in the sự kiện of emergency.
Blood components require filter tubing to remove clots, debris, and coagulated protein. A straight blood administration set is used for all transfusions (we no longer use Y’d blood tubing).Glass bottles containing albumin and IVIG require vented tubing.
If using a pressure infusion device, ensure it is safe to use with transfusions. Some infusion devices can cause mechanical hemolysis.
- 0.9% NS for RBCD5W for IVIG
Refer to blood product fact sheets for all other products.
If this is an elective transfusion, an alternate approach is to prime the IV administration set with the blood product just prior to administration.
7. Assess laboratory values to confirm rationale for transfusion. For example Hgb, hematocrit, coagulation values, platelent count. This ensures the transfusion is appropriate. 8. Check that the prescriber has obtained the necessary consent. It is the prescriber’s responsibility to obtain consent for blood or blood products. 9. The nurse confirms consent by ensuring the patient understands the procedure, rationale and by providing an opportunity for the patient’s concerns / questions to be answered.
9. The nurse confirms consent by ensuring the patient understands the procedure, rationale and by providing an opportunity for the patient’s concerns / questions to be answered. RN to document confirmation of consent.
Blood products require consent prior to administration.Notify the prescriber if patient is unable to provide indication of understanding the proposed blood or blood product transfusions.
10. Obtain and record the pre-transfusion baseline vitals including temperature, pulse, respirations, blood pressure, and SpO2.In addition, assess for other symptoms that may be confused with transfusion reaction.
Fever, rashes, flank pain, or shortness of breath may be preexisting and thus difficult to differentiate from a transfusion reaction.This assessment should be done within 30 minutes of initiating the transfusion. These serve as a baseline in which to compare any changes that may suggest transfusion reaction.
 11. Have emergency equipment available the bedside (oxygen, suction, etc.).
Be prepared for potential complications, as prompt intervention may be required to prevent serious complications.
11. Have emergency equipment available the bedside (oxygen, suction, etc.).
Be prepared for potential complications, as prompt intervention may be required to prevent serious complications.  Emergency equipment check bedside
12. Complete all documentation as required per agency policy.
Proper documentation provides evidence that all required procedures have been followed to prepare for a transfusion.
Emergency equipment check bedside
12. Complete all documentation as required per agency policy.
Proper documentation provides evidence that all required procedures have been followed to prepare for a transfusion. You have completed bedside check #1. You are now ready to call for the blood product.
Data sources: Alberta Health Services, 2015b; Canadian Blood Services, 2017c; Interior Health, 2022; Perry et al., 2022; Vancouver Coastal Health, 2008Checklist 76: Transfusion of Blood and Blood Products
Disclaimer: Always review and follow your agency policy regarding this specific skill. Safety considerations:- Blood and blood products cannot be mixed with any IV medicationsSpecific blood administration tubing is required for all blood transfusions. New tubing / filter is required after 4 hours.See agency policy for using EID for the administration of blood products. EIDs should have a sticker on them to indicate their safe use with blood products.Intravenous immunoglobulin (IVIG) is
only compatible with D5W.All blood products taken from the blood bank must be hung within 30 minutes and administered (infused) within 4 hours due to the risk of bacterial proliferation in the blood component room temperature. If the product cannot be infused within 4 hours, stop the transfusion and return the remaining blood component to the TMS.
 Figure 8.32 Blood product
example
4. Document any clinical sign or symptom that may be confused with a transfusion reaction (e.g., existing fever).
Serves as baseline to which further assessments can be compared.
5. Complete bedside check with two healthcare providers:
Figure 8.32 Blood product
example
4. Document any clinical sign or symptom that may be confused with a transfusion reaction (e.g., existing fever).
Serves as baseline to which further assessments can be compared.
5. Complete bedside check with two healthcare providers: Transfusionist: Leads and verbalizes all of the necessary elements.
2nd person verifier: Verbally confirms after each element is checked.
- Confirm prescriber’s order.Patient identification: Patient to state full name and DOB. Must be an exact match on patient facility ID and TMS documentsTMS ID band number (a.k.a. blood band)Blood
component: Read out the name of the component on the TMS document and the blood component container label.Patient ABO group: From the TMS documentsBlood component ABO group: From the TMS document and blood component container labelBlood component serial number: From the TMS document and blood component labelBlood component expiry date
 Confirm patient identity
Confirm patient identity TMS record
TMS recordIf there are any discrepancies, STOP the process and contact the TMS for resolution and direction. Do not proceed.
6. Perform hand hygiene. Decreases risk of transmitting microorganisms.Do not remove the product from the presence of the patient; prime bedside. If product is removed from bedside, the final verification process must be completed again.
7. Invert product 5 to 10 times and insert spike of the blood administration set into the blood product container.Squeeze the drip chamber.
Completely cover the filter with product. Fill the top of the drip chamber 1/2 to 1/3 full.

Priming blood tubing is very similar to priming IV tubing.
8. Initiate transfusion.Stay the patient’s bedside for the first 5 minutes ensuring the blood enters the patient’s circulation.
Obtain vitals after 15 minutes. Assess for other signs of reaction. If stable, increase transfusion rate as per orders or as per the nurse’s judgment of patient risk.
Advise patient on the signs and symptoms of transfusion reaction and what and when to report.
Adults: Initiate infusion as per agency guidelines. Infusions always start out slowly because most transfusion reactions occur within first 15 minutes of a transfusion. Infusing small amounts of blood component initially minimizes volume of blood to which patient is exposed, thereby minimizing severity of reaction.For example: Packed RBCs: 50 ml/hour for 15 minutes. Platelets / plasma: 50 to 100 ml/hour for 15 minutes
 Infusion of packed RBC
Infusion of packed RBCFor all units to be infused, remain with the patient for the first 5 minutes and assess for clinical signs of transfusion reaction.
Recommended best practice is to transfuse each unit of packed RBCs over 2 hours as long as no medical contraindications are evident OR as per prescribers’ orders.
9. Continue to monitor vitals signs q1h up to and including 1 hour post transfusion or until patient is stable.Ongoing patient assessment and monitoring is necessary.
 10. In the sự kiện of a transfusion reaction, stop the infusion.
10. In the sự kiện of a transfusion reaction, stop the infusion.
- Manage transfusion reactions as per agency protocol.Complete required transfusion reaction form.Return remaining blood to blood bank for further investigation.
Blood tubing must be discarded after 2 units or 4 hours, whichever comes first.
12. At the end of the transfusion, flush lines according to agency flushing protocol. CVCs often require 20 saline turbulent flush after a transfusion to maintain lumen patency. See agency flushing and locking protocols. 13. Discard waste in biohazard waste container. This prevents the spread of biohazard waste. 14. Complete all documentation as required by agency. Documentation may include:- Transfusion record formAll vital signs and reactionsAny significant findings, initiation and termination of transfusionRecord of transfusion on the in-and-out sheetBlood component tags filled out and returned to TMS
Checklist 77: Managing a Blood or Blood Product Transfusion Reaction
Disclaimer: Always review and follow your agency policy regarding this specific skill. Safety considerations:- Always review your agency’s algorithm for managing mild to severe reactions. For example, if a reaction is mild (e.g., fever), and without any other complications, a patient may continue the transfusion if monitored closely. Most other transfusion reactions require the transfusion to be stopped immediately.A blood transfusion reaction may occur 24 to 48 hours post-transfusion.
Each separate unit presents a potential for an adverse reaction.Follow emergency transfusion guidelines when dealing with an emergency blood or blood product transfusion.Be aware of which types of blood or blood products cause the most types of transfusion reactions.Be aware of the types of patients high risk for blood or blood product transfusion reactions.Always have emergency equipment and medications available during a transfusion. For example,
epinephrine IV should always be readily available.
IV access is necessary in the sự kiện emergency medications are needed.
3. Complete assessment including vitals signs, respiratory assessment, and which parts of the body toàn thân are affected (i.e., hives or rash). Assessment findings may inform the type and severity of reaction.Provide supportive measures as required (oxygen, etc.).
4. Report symptoms to prescriber for medical assessment, identification of type of reaction, and instructions for treatment. The prescriber responsible for the patient must be informed of all transfusion reactions. Treat signs and symptoms as ordered. 5. Frequent monitoring. Check vital signs every 15 minutes until stable. Frequent assessment helps to determine improved or worsening condition. 6. Check all labels, tags, forms, blood order, and patient’s identification band to determine if there is a clerical discrepancy. Clerical errors account for the majority of blood transfusion reactions. 7. Notify the TMS / lab to report the reaction and steps taken. Document as per agency policy. Notify TMS when any adverse reaction occurs, even if transfusion is continued. 7a. Allergic transfusion reactions (except anaphylaxis): TMS will determine need for further bloodwork. Transfusion may be resumed if:- Physician order to do so; ANDTransfusionist confirms ID with blood product tag and label as correct; ANDVigilant monitoring by transfusionist is possible; ANDProduct can be reasonably infused within 4 hours of issuance from TMS.
All blood products and IV tubing are investigated by the transfusion services and reported to Canadian Blood Services and Public Health Agency of Canada. These professional bodies are responsible for reporting and recording incidents of reactions.
8. Document as per agency policy. Document time, date, signs and symptoms, type of product, notification to the physician and management of reaction, and patient response to management of reaction. Documentation includes, but is not limited to:- Transfusion reaction formPatient chartReport for transfusion services (blood bank)Patient Safety Learning System (PSLS) report
Data Sources: Alberta Health Services, 2015a, 2015b; Canadian Blood Services, 2022; Interior Health, 2022;
Critical Thinking Exercises
How long can blood or blood products be room air temperature before being considered risk for infusion?You are about to initiate an infusion of packed red blood cells. What patient teaching is important to include about possible signs and symptoms of reaction?Attributions
Figure 8.31. Red Blood Cells from BCIT is used under a CC BY-SA 4.0 international license.
Figure 8.32 Blood Product Example by author is licensed under a CC BY-SA 4.0 international license.
Why is filtered tubing used during infusion of blood products?
Blood Infusion. Blood components must be filtered during transfusion to remove clots and small clumps of platelets and white blood cells that form during collection and storage.Can you use the same tubing for blood?
We use the same primary tubing for all units of blood hung in a 24 hour period. We do change the secondary filter with each unit that is hung.How often must you change the tubing for blood products?
Specific blood administration tubing is required for all blood transfusions. Blood tubing is changed every 4 hours or 4 units, whichever comes first. Tải thêm tài liệu liên quan đến nội dung bài viết What is special about the tubing used for administration of blood products? Blood transfusion filter Blood transfusion reactions Blood transfusion tubing
Post a Comment